NORFOLK, Va. — Porsche Richardson was diagnosed with breast cancer in 2022.
The Virginia Beach mother was 44 years old at the time. She was tested after finding a lump during a breast self-exam.
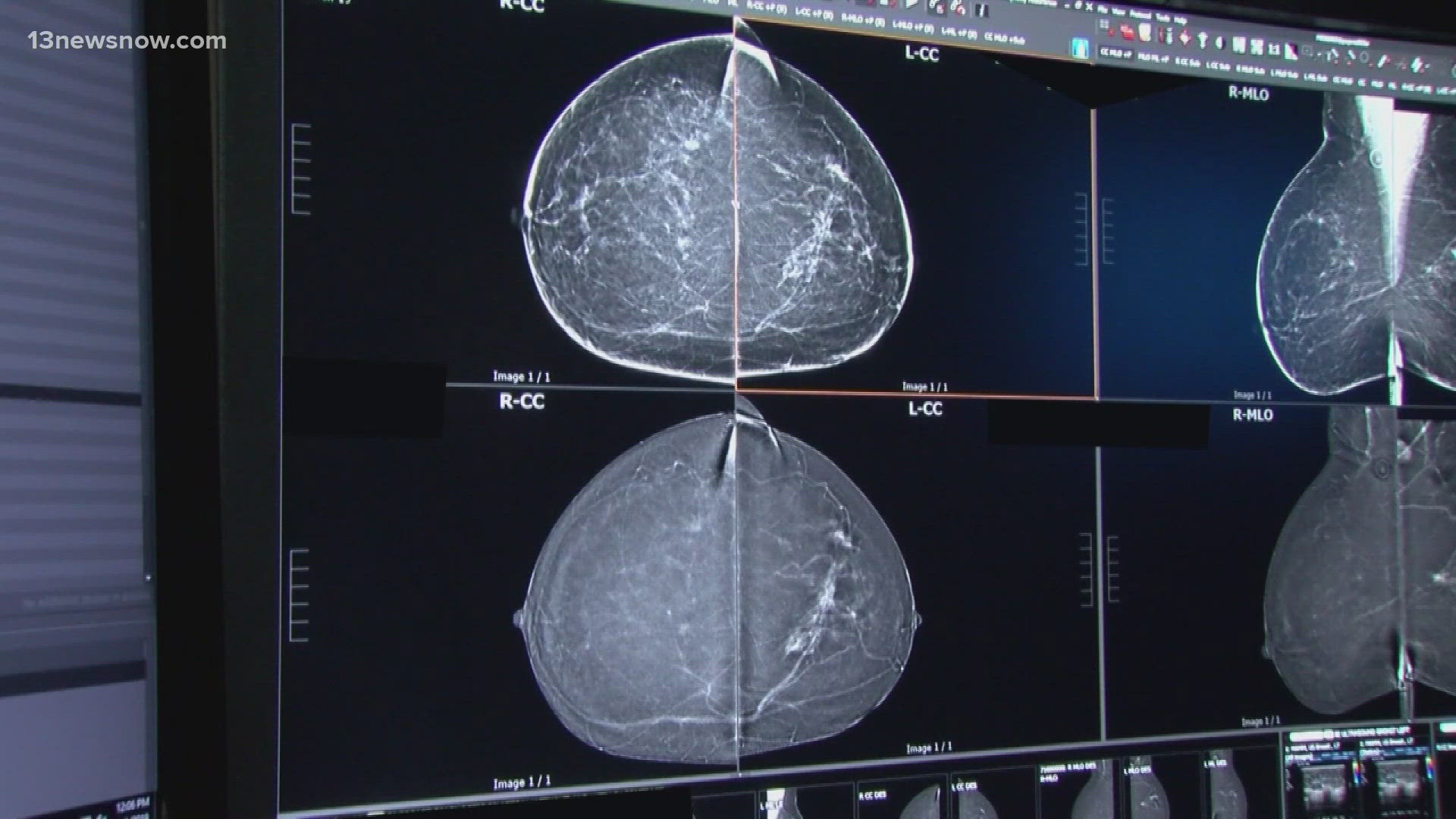
"I had a mammogram done in February, prior to my diagnosis, which came back completely normal," Richardson said. "And by June, I had a palpable mass."
While further testing eventually led to her diagnosis, Richardson credits routine cancer screenings with catching the disease early.
Recent data shows a 2% increase each year in breast cancer diagnosis rates among women in their 40s. To account for this, the United States Preventive Services Task Force -- a group of experts who provide preventive healthcare guidelines -- revisited its breast cancer screening guidance. Updates were drafted in May 2023, and a finalized version was released last week without major changes.
The new guidelines lower the recommended age to 40 for women of average risk to begin getting routine mammography screenings. Previously, the suggested age was 50.
However, the task force notes that if women have a personal history of breast cancer or breast lesions requiring one or more biopsies, are at very high risk following genetic testing, or had high-dose radiation therapy to their chest at a young age, they should consider screening at an even earlier age.
The American Cancer Society subsequently released a statement regarding the updated recommendations.
"The last time the [USPSTF] guidelines were updated was 2016," said Dr. Bruce Waldholtz, a national board member of the ACS Cancer Action Network. "And a lot has gone on and the science has changed and women's risk has changed during that time."
Dr. Waldholtz said the task force's lowered recommended age aligns with breast cancer screening guidance from ACS, but the two groups differ on other recommendations.
"The task force guidelines recommend stopping screening at age 75," Dr. Waldholtz said. "The American Cancer Society guideline is if a woman reaches age 75 and still has 10 years of expected life expectancy... to continue screening."
For women 75 and older, USPSTF still recommends that they talk to their doctor about whether to continue screening, based on their preferences and medical history.
The task force and ACS also differ in their guidance for how often women should be screened.
"The American Cancer Society recommends screening annually, every year, from age 45 to 55, in that group, for all women," Dr. Waldholtz said. "And the [USPSTF], the task force, recommends every other year screening."
However, Dr. Waldholtz notes that there is some overlap in frequency guidance from the two organizations.
"The ACS guidelines from 40 to 45 recommend that women consider screening... and that from 55 onward, that women be screened every other year," Dr. Waldholtz said. "So, from 55 to 75, the two guidelines are aligned exactly."
The updated guidelines from USPSTF also aim to address racial disparities in breast cancer rates.
"Black women have a 40% higher chance of dying from breast cancer," Dr. Waldholtz said, noting that the updated guidance aim to detect breast cancer in women earlier. "If a 40-year-old has a mammogram and there's an abnormality, and a case of advanced cancer is prevented, you've extended that woman's life by many years."
There are calls for more research on breast cancer risk and outcomes in Black women. This week, the American Cancer Society launched VOICES of Black Women, a national study of cancer and other health conditions among Black women.
The goal is to enroll at least 100,000 Black women in the U.S. between ages 25 and 55 who have never had cancer. Participants will complete online health surveys twice a year for at least 30 years.
"This is the largest study of its type in the world," Dr. Waldholtz said. "This study will occur in states that involve 90% of where African American women live."
Enrollment is open across nearly two dozen states, including Virginia and North Carolina.
Meanwhile, USPSTF is also calling for more research of dense breast tissue, which the task force notes nearly half of all women have.
"Women now are going to be receiving notice that, on their mammogram, they had dense breasts," Dr. Waldholtz said. "It makes it harder to see on the mammogram itself."
Dr. Waldholtz believes the key takeaway of the task force's update is that cancer screenings save lives.
Richardson said women should be proactive in talking to their doctor about their personal risks and getting regular cancer screening.
"Continue to be the squeaky wheel, you know, until you are heard and you are able to get tests done," Richardson said.
She also recommends women conduct breast self-exams and build trust with their medical team.
The task force's updated recommendation will not impact insurance coverage. But, by law, mammograms should be covered by insurance for all women ages 40 and older.